Amoebic Meningoencephalitis in Kerala
About the Disease
-
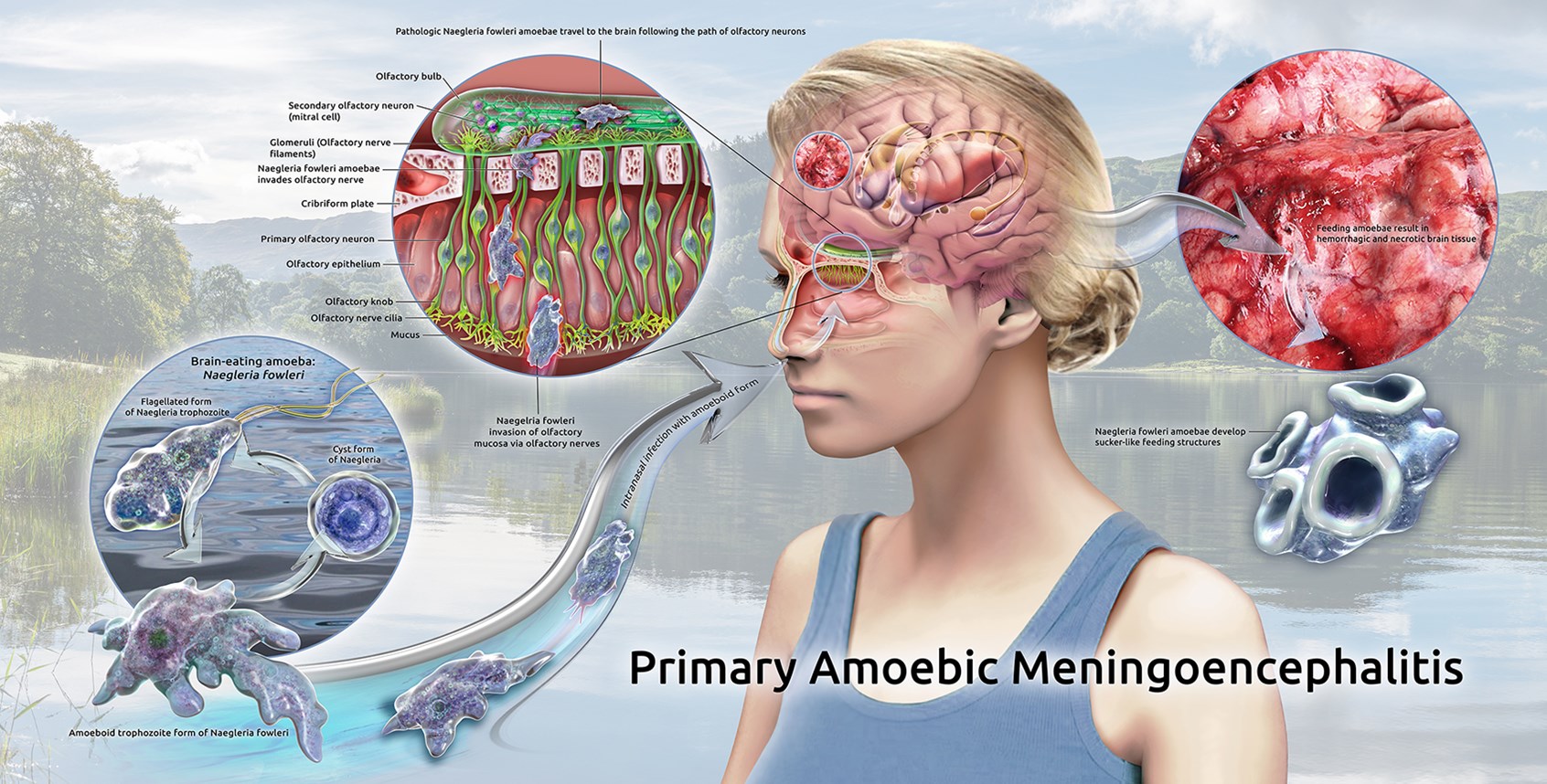
Amoebic meningoencephalitis – rare, often fatal brain infection caused by free-living amoebae in freshwater (ponds, lakes, rivers, wells).
-
Two types:
-
PAM (Primary Amoebic Meningoencephalitis) – caused by Naegleria fowleri (“brain-eating amoeba”), rapid onset, high fatality.
-
GAE (Granulomatous Amoebic Encephalitis) – caused by Acanthamoeba spp. and others; symptoms mimic meningitis/encephalitis/brain abscess.
-
-
Symptoms: fever, vomiting, stiff neck, confusion; rapid deterioration if untreated.
Recent Cases in Kerala
-
Reported in Kozhikode, Malappuram, Wayanad, Kollam, Thiruvananthapuram districts.
-
Example:
-
Anaya (Class IV student), died Aug 14, 2025, after bathing in a pond.
-
Her brother and a 3-month-old also infected.
-
Malappuram: 14 cases, 4 deaths in 2025.
-
-
Clusters rare – most are sporadic cases.
Causes and Risk Factors
-
Naegleria fowleri thrives in warm, stagnant freshwater.
-
Feeds on bacteria and algae; risk rises with faecal contamination (coliform bacteria).
-
Infection occurs when contaminated water enters the nasal cavity (esp. in children due to porous cribriform plate).
-
Climate change → rising temperatures favour amoebic growth.
-
Risk sites: ponds, unchlorinated wells, stagnant village tanks, religious rituals where water dripped into nose.
Public Health Response
-
Early challenges: until 2023, almost all patients succumbed due to late diagnosis.
-
From 2024:
-
Kerala issued diagnosis & management guidelines.
-
Patients with meningitis-like symptoms asked about freshwater exposure (past 14 days).
-
Cerebrospinal fluid (CSF) tested for amoebae.
-
Miltefosin (anti-parasitic drug) added to multi-drug therapy → survival rate improved dramatically (14 of 19 cases survived in mid-2024).
-
Community Action & Awareness
-
Ponds closed / warning boards: e.g., Navaikulam panchayat put flex boards on ~40 ponds (2024).
-
Cleaning drives: ponds cleaned, chlorinated, reopened once safe.
-
Case studies:
-
Some children recovered with early treatment (Navaikulam).
-
Others face long-term health issues (Kollam case).
-
-
State initiative: Intensive cleanliness drive (Aug 30–31, 2025) with local bodies, Haritha Kerala Mission, Water Resources Dept.
Preventive Measures
-
Chlorinate wells, ponds, tanks regularly.
-
Avoid letting water enter nose during bathing, swimming, rituals.
-
Keep overhead tanks clean.
-
Public health messaging: awareness without panic.
Key Takeaways
-
Kerala is epicentre of reported PAM/GAE cases in India since 2016.
-
Climate change + poor sanitation = rising threat.
-
Early diagnosis + miltefosin therapy can save lives.
-
Waterbody management & public awareness are crucial preventive strategies.
-
Rare disease but high fatality rate makes even a few cases a public health concern.
Meningitis and Encephalitis are the two main kinds of neurological conditions related to the brain and spinal cord, where the layer surrounding the brain or the brain itself gets inflamed.
Meningitis vs. Encephalitis
| S.N. | Character | Meningitis | Encephalitis |
|---|---|---|---|
| 1 | Definition | Inflammation of the thin membranes surrounding the brain & spinal cord (meninges – pia mater & arachnoid mater). | Inflammation of the brain parenchyma. |
| 2 | Causative Agent | Bacteria, viruses, fungi. | Mostly viruses. |
| 3 | Microorganisms involved | - Viruses: echovirus, poliovirus, coxsackie. - Bacteria: Streptococcus, Neisseria, Haemophilus, Listeria etc. | - Viruses: herpes, rabies, arboviruses, cytomegalovirus. - Bacteria: meningococci, pneumococci, Haemophilus, TB bacteria. - Fungi/parasites: leptospirosis, toxoplasmosis, trichinellosis. |
| 4 | Other Causes | - Brain tumor reaction - Post-chemotherapy - Lead poisoning - Contrast medium reaction - Parasites, fungal infections | - Complicated brain tumors - Sarcoidosis - Leukemia - Multiple sclerosis - Lead poisoning - Reactions to injected substances - Cerebrovascular accidents |
| 5 | Incubation Period | Symptoms develop within hours → 2 days. | 3–5 days (most common). |
| 6 | Symptoms | Headache, vomiting/nausea, skin rash or discoloration, high fever, stiff neck, confusion, double vision. | Headache, joint pain, irritability, fever, lethargy, seizures, behavioral changes. |
| 7 | Complications | - Hearing/vision loss (temporary/permanent) - Irreversible brain damage (cognition, movement) - Hydrocephalus - May lead to encephalitis | - Memory issues - Personality/behavioral changes - Speech problems - Epilepsy - Physical/motor deficits - Depression/low mood - Fatigue |
| 8 | Rash | May be present (skin rash/discoloration). | Absent. |
| 9 | Altered Mental Status (AMS) | Usually no focal deficits or AMS. | Altered mental status common. |
| 10 | Forms | Only one form (meningeal inflammation). | Two forms: - Primary: brain/spinal cord directly affected. - Secondary: spreads from infection in another organ. |
| 11 | Types | Tuberculous, aseptic, syphilitic, cryptococcal, staphylococcal, Gram-negative, pneumococcal, H. influenza, meningococcal. | - Polyoencephalitis (gray matter) - Leucoencephalitis (white matter) - Panencephalomyelitis (gray + white matter) - Perivenous encephalomyelitis |
| 12 | Modes of Transmission | (Depends on agent) – Mainly droplet infection (bacteria in nose/mouth discharges). | - Respiratory droplets - Skin contact - Insect bites (mosquito, tick, horse tick) - Migratory birds - Contaminated food/water |
