Vitamin D deficiency linked to neurodevelopmental issues
A major Danish study, published in The Lancet Psychiatry, links low neonatal vitamin D levels to an increased risk of schizophrenia, ADHD, and autism. Using dried blood spot samples from over 88,000 individuals born between 1981 and 2005, researchers found:
-
Higher vitamin D levels at birth reduced risks:
-
18% lower risk of schizophrenia
-
11% lower risk of ADHD
-
7% lower risk of autism
-
-
No link was found with depression or bipolar disorder, likely due to their later onset.
The research team measured 25-hydroxyvitamin D [25(OH)D], the standard biomarker of vitamin D status, and vitamin D-binding protein, which transports vitamin D in the bloodstream and extends its biological activity.
Genetic Evidence:
Researchers used:
-
Polygenic Risk Scores (PRS) to indicate inherited vitamin D levels
-
Mendelian Randomisation to establish possible causality
These tools suggested a biological link, especially for ADHD, though confounding factors and pleiotropy (genes affecting multiple traits) remain concerns.
Maternal Vitamin D and Foetal Health:
During pregnancy, a mother undergoes hormonal and metabolic adaptations to supply calcium for foetal skeletal development—especially during the third trimester. These include:
-
Increased intestinal calcium absorption,
-
Higher renal calcium excretion,
-
Doubling of active vitamin D levels.
However, maternal vitamin D levels do not rise adequately unless supported by improved sunlight exposure or dietary intake, making deficiency common even in well-nourished Indian pregnancies.
A 2024 study in Bundelkhand showed a strong positive correlation between maternal and infant vitamin D levels, indicating that deficiency is inherited across generations.
This highlights vitamin D insufficiency as a biological legacy, affecting not just bone health, but potentially brain development as suggested by recent studies.
Limitations:
-
Vitamin D was measured only at birth, not throughout pregnancy.
-
A 2024 Danish trial found no effect of supplementation from week 24 on later autism/ADHD — suggesting timing and deficiency status matter.
-
Study participants were mostly European, so findings may not fully apply to diverse populations.
India-Specific Findings:
Despite abundant sunlight, vitamin D deficiency is widespread in India:
-
74% of infants and 85.5% of mothers at AIIMS Rishikesh were deficient.
-
A Bengaluru study found 92.1% newborns deficient.
-
Vitamin D levels don’t rise during pregnancy without dietary/supplemental support.
A 2024 Indian study showed a strong correlation between maternal and infant vitamin D levels, underscoring the intergenerational transmission of deficiency.
"Vitamin D constitutes a form of biological inheritance transmitted across generations, significantly influencing skeletal health by ensuring proper bone development and preventing disorders such as rickets in children."
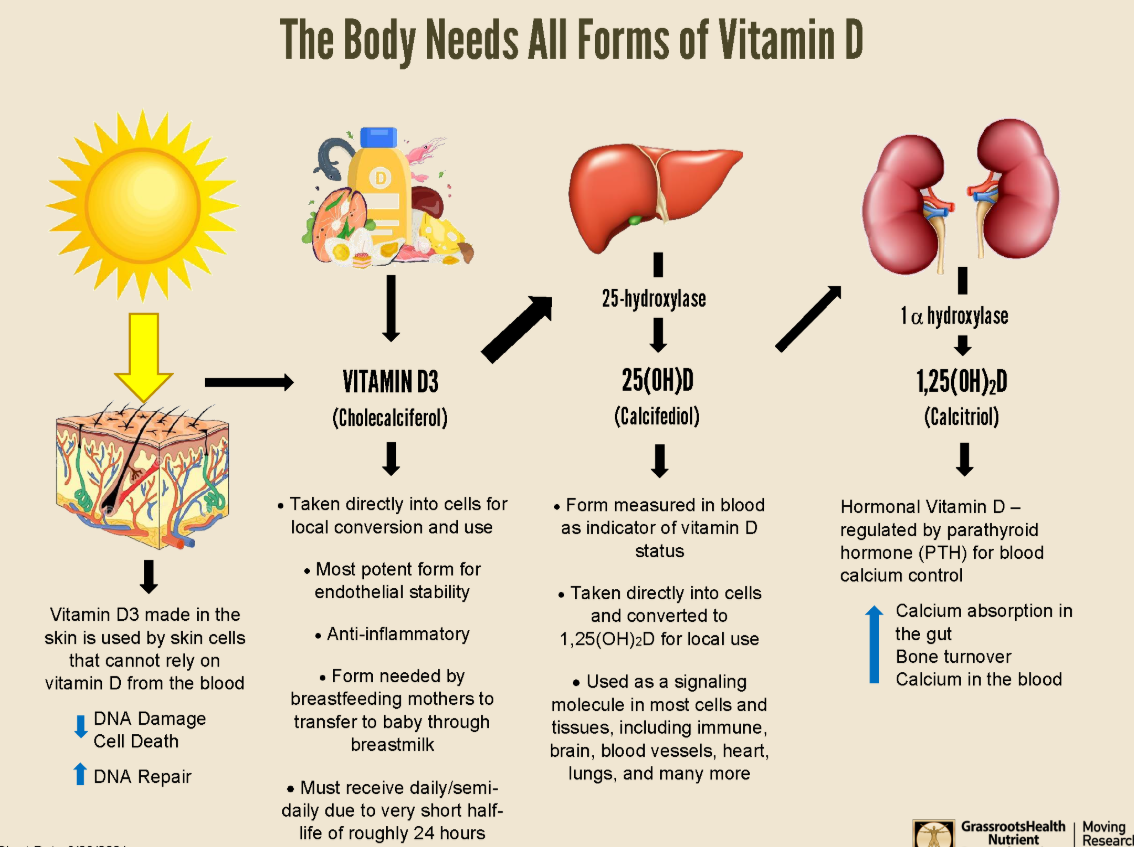
Vitamin D3 (Cholecalciferol):
-
Main source: Synthesized in skin via UVB sunlight; minor dietary sources include fatty fish, eggs, dairy, and fortified foods.
-
Skin production: Skin cells (keratinocytes) must synthesize their own vitamin D3.
-
Functions:
-
Enters blood and is delivered to all body tissues.
-
Helps DNA repair, reduces UV-induced skin damage, and fights infections, autoimmune diseases, and inflammation.
-
Can cross placenta and is transferred via breast milk if maternal levels are adequate.
-
-
Potency:
-
1000× more potent than 25(OH)D, and 10× more than 1,25(OH)2D.
-
-
Half-life: ~24 hours.
25-hydroxyvitamin D [25(OH)D / Calcifediol]:
-
Primary circulating form, formed by hydroxylation of vitamin D3 in the liver.
-
Measured in blood to assess vitamin D status.
-
Functions:
-
Taken up by immune, brain, heart, and other cells.
-
Precursor to the hormonal form (1,25D).
-
Modulates T-cell activation and acts as a local signaling molecule.
-
-
Half-life: ~2–3 weeks.
-
Clinical relevance: Can be supplemented directly in immune emergencies (e.g., COVID-19).
1,25-dihydroxyvitamin D [1,25(OH)2D / Calcitriol]:
-
Hormonal and most active form, formed mainly in kidneys from 25(OH)D via parathyroid hormone (PTH) regulation.
-
Functions:
-
Regulates intestinal calcium absorption and bone turnover.
-
Also synthesized locally in cells during immune responses (paracrine function).
-
-
Half-life: ~4 hours.
